|
Issue #5: January 20113
Carpal Tunnel Syndrome!
By: Robert O’Leary, DO, and Ricardo A. Nieves, M.D.
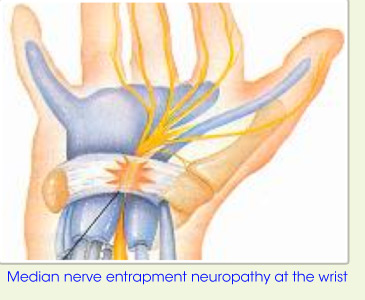
The most commonly pinched nerve or so called entrapment neuropathy is the Median nerve at the wrist which is called Carpal Tunnel Syndrome (CTS). The name for wrist in Latin is Carpal and the median nerve travels through the wrist in a tunnel and the term Carpal Tunnel Syndrome is pinched median nerve at the wrist.
 Patients with Carpal Tunnel Syndrome present with pain, numbness, tingling and weakness into the hand and fingers (thumb, index finger, middle finger and radial half of the ring finger). The symptoms can be present at night causing the person affected to shake out their hands for relief. This is a rather telling way to help diagnose the problem and is called "Flick Sign". Patients with Carpal Tunnel Syndrome present with pain, numbness, tingling and weakness into the hand and fingers (thumb, index finger, middle finger and radial half of the ring finger). The symptoms can be present at night causing the person affected to shake out their hands for relief. This is a rather telling way to help diagnose the problem and is called "Flick Sign".
About 5% of the population gets Carpal Tunnel Syndrome.
It affects women 3 times more commonly than men, perhaps due to having smaller wrists/carpal tunnels. 50% of the time CTS involves both hands.
CTS has being previously associated with sustained or repetitive bending of the wrist, trauma to the wrist, diabetes, thyroid disease, obesity, rheumatoid arthritis, pregnancy and vibration. Recent literature review recognized vibration exposure as a risk factor and repetitive typing or use of the extremity is no longer seen as a cause.
In a Danish study, published in the Journal of the American Medical Association in 2003, found that workplace computer use does not pose a risk of developing carpal tunnel syndrome. And a 2001 study in Neurology of computer users at a medical facility found that heavy computer use (up to seven hours a day) did not increase a person's risk of developing carpal tunnel syndrome. Repetitive use of the mouse for more than 4 hours might still be a risk factor.
In a systematic literature review by Keith T. Palmer et al (Occ. Med., 2007) found reasonable evidence that regular and prolonged use of hand-held vibratory tools increases the risk of CTS >2-fold and found substantial evidence for similar or even higher risks from prolonged and highly repetitious flexion and extension of the wrist, especially when allied with a forceful grip. The balance of evidence on keyboard and computer work did not indicate an important association with CTS.
It is Safe to use a Keyboard, Whenever and Wherever You Wish, JAMA 2003; 289 (22): 2963
Neurology 2001; 56 (11):1568-70, Occ & Environ Med 1997; 54 (10): 734-740, JOEM 1996; 38 (5): 469-484, JOEM 1996; 38 (11): 1079-1084, Arch Environ Health 1996; 51 (5): 395-407, Hand Clinics 2002; 18: 211-217
Keyboard Redesign, No decrease CTS, JOEM 1999; 41: 111-119, Am J Prev Med 2000; 18: 37-50
Carpal tunnel syndrome and the use of computer mouse and keyboard: A systematic
Review, BMC Musculoskeletal Disorders 2008, 9: 134. Conclusion: There is insufficient
Epidemiological evidence that computer work causes CTS.
Maine Prospective Carpal Tunnel Release Study, Katz, et al. Determinants of Work Absence Following Surgery for Carpal Tunnel Syndrome., Am J Industr Med 2005; 47: 120-130. 181 out of 241 patients available for 6 & 12 month follow up. 57% of patients were in Workers’ Comp System. If no attorney, 19% still off work at 6 months and 23% off work at 12 months. If Attorney Involved, 53% still off work at 6 months and 40% off work at 12 months.
In a major study published by NCCI in April of 2005, we learn that carpal tunnel in the comp system ranks second among major lost time diagnoses - second only to lower back strain. Sixty per cent of carpal tunnel claims lead to lost time - compared to only 34 per cent for lower back strains. The older people get, the more likely that their carpal tunnel will be treated with surgery - and where surgery is the treatment, the costs are three times higher.
In the workers’ compensation patients it is very important to establish causation by obtaining a detailed history (including work and recreational activities), obtaining a physical examination with findings consistent with CTS and confirming the diagnosis with Gold Standard Electrodiagnostic Studies.
The Emg/ Ncs (Electrodiagnostic Study) needs to be completed by a provider trained and experienced in performing and interpreting the study (Physical Medicine and Rehabilitation and/ or Neurology). Absolute values need to be obtained as per 6th Edition AMA Guides to the Evaluation of Permanent Impairment . For Carpal Tunnel Syndrome criteria include:
- Distal motor latency longer than 4.5 milliseconds for an 8 cm study
- Distal Peak sensory latency longer than 4.0 milliseconds for a 14 cm distance
- Distal peak compound nerve latency of longer than 2.4 milliseconds for transcarpal or midpalmar study of 8 cm
- Upper limb temperature must be stated in the report and must be at least 32 degrees Celsius for the study to be valid.
The electrodiagnostic study is also helpful in determining the severity of the condition (mild, moderate , severe), recent onset versus chronic, and ruled out other conditions such as cervical radiculopathy, brachial plexopathy, peripheral neuropathy and multifocal motor neuropathy.
CTS is treated by addressing the causative factors, wearing a splint on the wrist at night for two weeks, rest, taking medication, hand therapy, adaptive tools/devises in the home, injections and surgery as a last resort if patient fails conservative treatment and no surgical contraindications. Prevention is always the best treatment!
Relative risk of a poorer result with Carpal Tunnel Release in the Workers’ Compensation System compared to the same Surgery in the Health Insurance System is 4.24 (I Harris, et al.,
JAMA 2005; 293 (13):1644-1652).
Therefore, it is important to treat Carpal Tunnel Syndrome non surgically through preventions by keeping the wrists in a neutral position as possible, taking breaks and varying tasks, relaxing one's grip, staying warm and doing carpal tunnel stretching exercises.
Next month newsletter on Functional Capacity Evaluation
About the authors:
Robert O’Leary, DO, FAAPMR
 Dr. O’Leary is a musculoskeletal and neuromuscular specialist with advanced training and experience using the latest technologies such in Electrodiagnostic testing for carpal tunnel, sciatica and peripheral neuropathy as well as musculoskeletal ultrasound guided injection tendon, joint and spine procedures. With over twenty years of medical experience, Dr. Robert O'Leary began his practice in SWFL in 2007 and has built a large referral base through his patients' word of mouth due to his compassionate care and medical expertise. Dr. Robert O'Leary provides cares for many patients who believe that they have exhausted every medical treatment option without success. Physical Medicine integrates the finest parts of orthopedics and neurology and enhances them with Rehabilitation toward functional solutions. When complemented with his Pain Medicine training, experience and board certification a comprehensive medical assessment and treatment regime is appreciated beyond an ordinary evaluation. Dr. O’Leary is a musculoskeletal and neuromuscular specialist with advanced training and experience using the latest technologies such in Electrodiagnostic testing for carpal tunnel, sciatica and peripheral neuropathy as well as musculoskeletal ultrasound guided injection tendon, joint and spine procedures. With over twenty years of medical experience, Dr. Robert O'Leary began his practice in SWFL in 2007 and has built a large referral base through his patients' word of mouth due to his compassionate care and medical expertise. Dr. Robert O'Leary provides cares for many patients who believe that they have exhausted every medical treatment option without success. Physical Medicine integrates the finest parts of orthopedics and neurology and enhances them with Rehabilitation toward functional solutions. When complemented with his Pain Medicine training, experience and board certification a comprehensive medical assessment and treatment regime is appreciated beyond an ordinary evaluation.
Bonita Community Health Center
3501 Health Center Blvd.
Suite 2200
Bonita Springs, FL 34135
(239) 390-9778
www.DoRehab.com
|



